Need Help?
We are here to help.
We care for each one who come to us with hope in their hearts.

Men with absent sperms, very low sperms or in immotile sperms in semen can become father through intra-cytoplasmic sperm injection (ICSI) if sperm can be retrieved from their epididymis or testis.
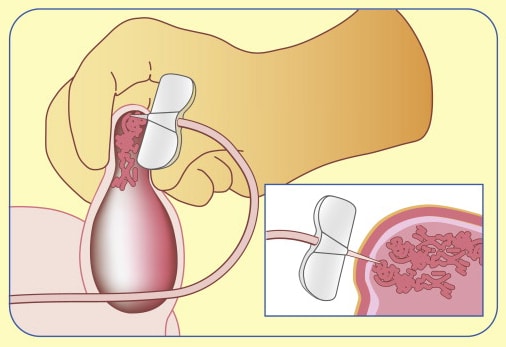
It uses surgical microscope to retrieve sperms from epididymis (the tube through which sperm travel after leaving the testicle) under magnification done in general anaesthesia. If moving (motile) sperm are seen, the fluid is taken for immediate use or frozen for future use.
It can be done under local anesthesia. In this technique, the sperms are retrieved from epididymis through multiple pricks and fewer sperm are collected. With PESA, there are sometimes not enough sperm to freeze for later use.
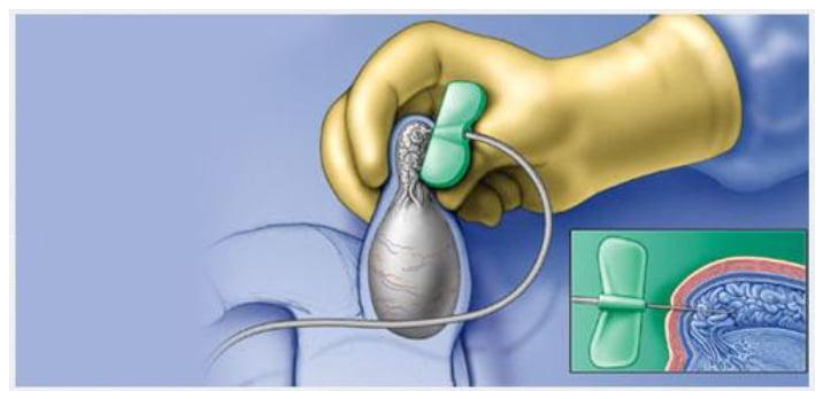
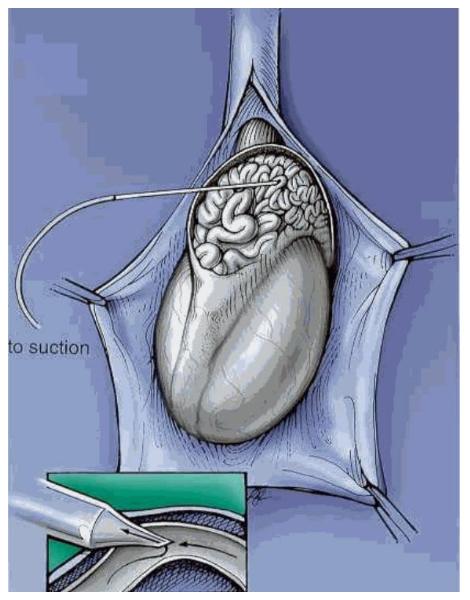
Sperm can be taken directly from the testicle when there are no sperm in the epididymis and in cases of nonobstructive azoospermia. A needle is inserted (aspiration) or a tissue (biopsy) is taken through the skin which provides more amount of sample to retrieve sperms.
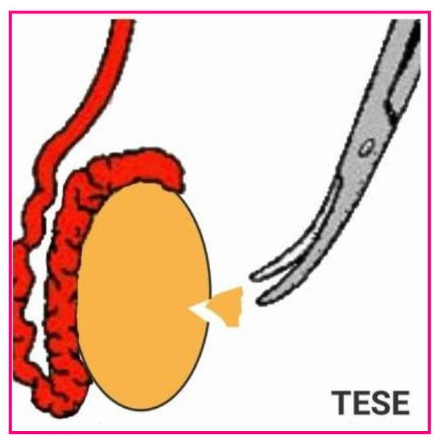
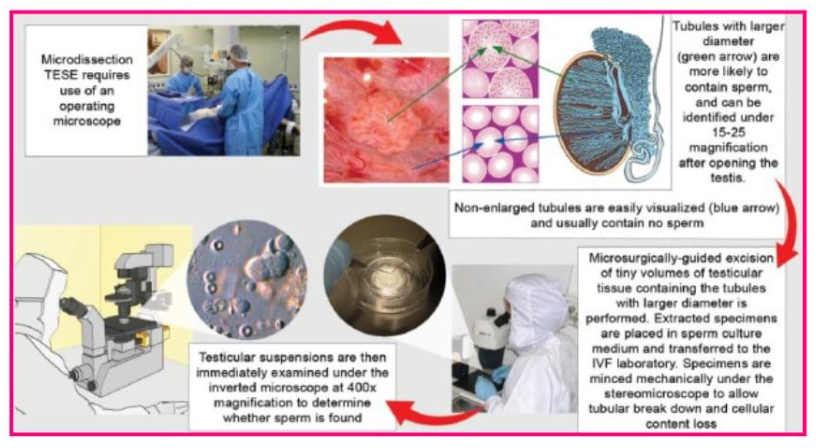
Open testicular sperm extraction can be done with an operating microscope (microsurgical). The microsurgical technique has higher sperm retrieval rates than the conventional method. Sperm have been found with microsurgical TESE even when sperm production by the testicles is very low. Major advantages of using the micro TESE technique are the lower chance of injury to the testicular blood supply, less loss of testicular tissue, and less blood in the biopsy specimen.
This technique is used for men who are unable to ejaculate voluntarily due to spinal cord injuries or other medical conditions. It involves applying electrical stimulation to the nerves in the rectum to induce ejaculation. The ejaculated semen is then collected for further use.
Varicocelectomy is a surgical procedure performed to treat a condition called varicocele, which is the enlargement of veins within the scrotum. This procedure aims to improve sperm production and fertility in men affected by varicoceles.
Varicocelectomy can improve sperm count through various mechanisms:
It helps in enhanced blood flow, testicular cooling, hormonal balance and reduction of oxidative stress.
There are a few different techniques used for varicocelectomy, including:
The choice of technique depends on various factors, including the surgeon’s expertise, the severity of the varicocele, and the patient’s specific condition. Each technique has its advantages and considerations, and the choice should be made after a thorough discussion between the patient and the healthcare provider.
Varicocelectomy is usually indicated when there is a Gd4 varicocele or palpapable varicocele associated with oligoasthenospemia and infertility. Whether varicelectomy increases sperm parameters and whether these improved paprameters help in getting the woman pregnant is debatable. It is argued that it may be better and less invasive to proceed to IVF with ICSI . Some studies have indicated that in en with very poor sperm parameters and repeated failed ICSI attempts associated with a palpable or Grade 4 varicocle, varicocelectomy may improve ICSI pregnancy rates.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2658802/
Reversal of Vasectomy is a surgical procedure performed to restore fertility in men who have previously undergone a vasectomy. The procedure involves reconnecting the vas deferens, the tubes that carry sperm from the testicles to the urethra, which were previously severed or blocked during the vasectomy. There are two main techniques used for vasectomy reversal:
The choice between vasovasostomy and epididymovasostomy depends on various factors, such as the presence of sperm in the fluid within the vas deferens, the quality of the vas deferens, and the presence of any blockages or scarring in the epididymis. The surgeon will make a decision during the procedure based on the specific circumstances and the best chance of success.
It’s important to note that while vasectomy reversal is a viable option for restoring fertility, it is not always successful. Success rates depend on various factors, including the length of time since the vasectomy, the presence of scar tissue, and the overall health and fertility of the male partner. It is sometimes advisable to go ahead directly with IVF/ICSI.
We care for each one who come to us with hope in their hearts.

Disclaimer – Dr Kaberi is not associated with any Hosptial/Clinic other than “Advanced Fertility and Gyne Center (AFGC)”. AFGC has only four centers at present 1. “Lajpat Nagar” 2. “CR Park Delhi” 3. “Noida” 4. “Gurgaon“.