Need Help?
We are here to help.
We care for each one who come to us with hope in their hearts.


Polycystic Ovary is a condition where excess androgens (the male hormone) and excess insulin is present in the body. It can be genetic or because of lifestyle factors. Insulin resistance that is inherent in PCOS leads to increased chances of getting diabetes in future. Excess androgen displays symptoms including thick hair growth on the face and excessive acne. A combination of polycystic ovaries, androgenic symptoms and menstrual irregularity is known as PCOS.
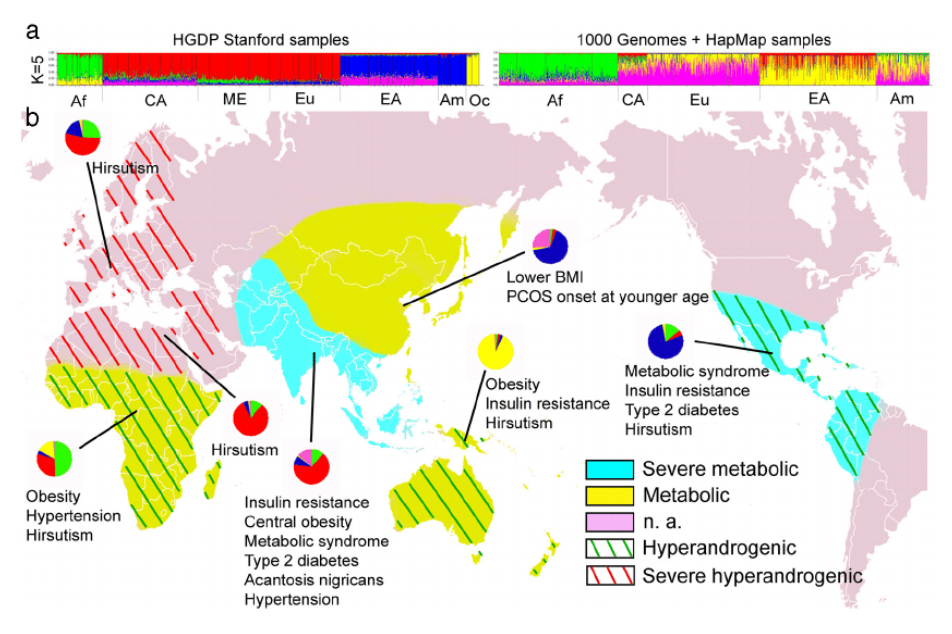
Now 10% of the women of child bearing age are estimated to have PCOS and less than < 50% of them are properly diagnosed, so, a lot needs to be done in that field. This is the world map and you will see India as the blue area and there is severe metabolic syndrome. PCO is associated with metabolic syndrome, which means it could lead to obesity, diabetes, skin problem, so this is very much common in South East Asia and PCOS presence in different form in different part of the globe. We see couples and women with different ethnic origin in our clinic. South East Asia, Indian, Pakistani, Bangladeshi have increased adiposity, insulin resistance, diabetes and metabolic risks . Caucasian have the mild phenotype and the east Asians that is from Japan, Korea and China have lower BMI and milder hirsutism. Africans have higher body mass, they are more obese, there metabolic feature are also high.
The basic diagnosis initially used to be called the Rotterdam criteria. It indicated a body with female reproductive organs displayed irregular periods cycles (lasting more than 31 days) or late periods (and negative pregnancy test). Excess androgen symptoms like balding, facial hair, pimples or acne were also observed.
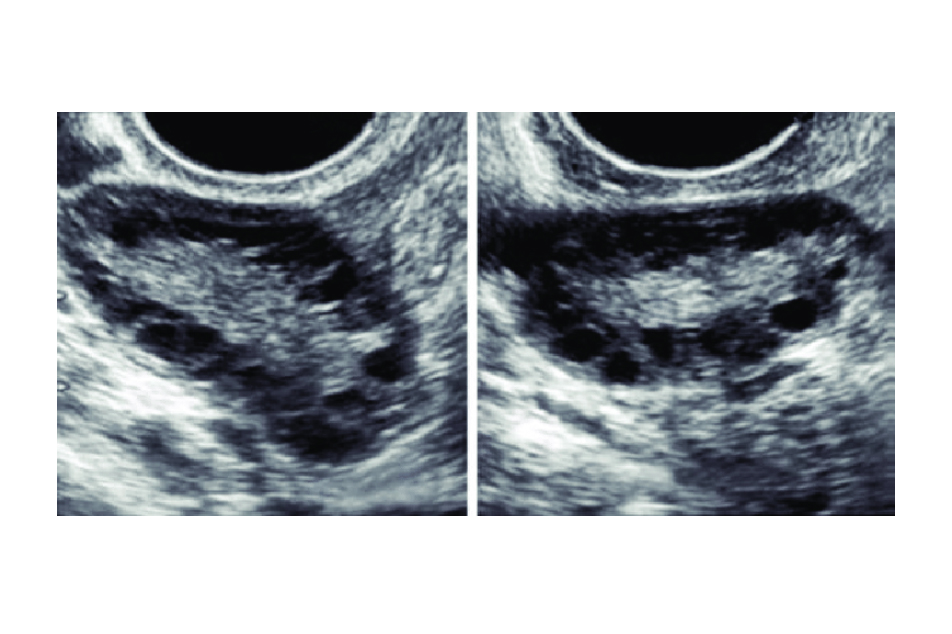
In 2018, International evidence based guidelines were issued. They concluded that if you have irregular cycles, and if you have acne or hair on your face that is indicative of hyper-androgenism you are diagnosed with PCOS. Blood test results showing increased testosterone is also taken as a positive indication of PCOS. Upon ultrasound, polycystic ovaries can be seen, confirming the diagnosis and thus marking the begining treatment of PCOS in India.
https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Polycystic-Ovary-Syndrome
The following conditions can minic PCOS:
At Advanced Fertility Clinic, we conduct thorough tests and analysis to understand your health condition. Once it has been established by our experts that you indeed show signs of PCOS, our experts will follow due course of treatment of PCOS in India.
The ultrasound conducted for examining the uterus for PCOS usually shows multiple cysts. A transvaginal probe might be required to confirm the test results. Our experts take up to 10-15 follicles each ovary and the volume of each ovary being more than 10 ml. It is noteworthy that transabdominal scans are not enough for the diagnoses of PCOS.
Though PCOD and PCOS can almost be used interchangeably, there are minor variations.
PCOD or Polycystic Ovarian Disorder: A medical condition which is caused by hormonal imbalance. In this condition the excessive male hormone secretion affects the ovaries leading to immature or partial mature egg formation, eventually leading to cyst formation. This condition can be genetic or due to environmental or lifestyle factors.
The condition is usually correctable and affects the fertility of a woman to a mild to moderate degree. Women with such condition can get pregnant naturally by just doing some modifications in their diet and lifestyle.
One can identify PCOD by understanding their symptoms like:
Ultrasound and blood tests are required to confirm the condition.
PCOS or Polycystic Ovarian Syndrome: On the other hand, along with increased body hair, weight gain and irregular periods is also associated with metabolic syndrome. It is difficult to get pregnant in PCOS due to irregular ovulation cycles.
The symptoms of PCOS may include:
PCOS is not a permanent condition. Through care and following a strict exercise and diet routine, you can achieve good health while reducing the effects of PCOS.
Here are few tips to follow:
At Advane Fertility Clinic, we aim at offering treatment of PCOS in India that is backed by modern science practices coupled with medication cycles that have a positive impact on the body. We aim at targeting the root causes of PCOS to provide a solution that is long lasting and easy to maintain.
Regarded as best doctor for PCOS in Delhi, we have helped many women reverse and manage their PCOS conditions and be able to conceive (either naturally or through our assistance). If you think PCOS is the end of your dreams to become a mother, you are wrong. Speak with our team of best doctor for PCOS in Delhi today and discuss your possibilities.
The most important is lifestyle measure, like correct diet and exercise. These are the main parameters in this. You have to maintain a healthy weight. You have to lose at least 5-10% of your excess weight -that much itself will cause a significant improvement in your symptoms. Weight-loss targets we all know how frustrating it can be for us and for our patients. There is a SMART way of weight loss. Specific, Measurable, Achievable, Realistic and Timely. You have to say you are 68 you become 62, specific, measurable you can measure it, achievable. You know 90kg lady you say come back in 60kg is not possible. Realistic, timely, set timelines like in 1-2 months, you have to lose this much. So the smart way of losing weight is very important and along with this your assertiveness, slow eating, cognitive behavior monitoring because you know is like a stimulus, you could be stress eating , so behavioral eating need to be in place and usually if you are <500 calories for your daily dietary intake ,so roughly for women it comes to 1200-1500 kcal is what is advised and less of whites, like sugar, less of carbohydrates, more of fruits, vegetables and proteins what is usually advised. Exercise is very important and in this if you want to lose weight moderate intensity and vigorous intensity per week moderate is 4 hrs per week and 2 hrs of vigorous in a week and muscle strengthening at least twice in a week. All your muscles, upper body, lower body, hands, legs, so it has to be regimen that a physiotherapist and a weight trainer can help.
The medical management which can be ovulation induction drugs, because these women do not ovulate regularly, they have early or delayed cycle., so you give medication that make the follicle mature and release the egg called ovulation induction agents. Nowadays the first choice is letrozole. Clomiphene citrate also a good drug, you can combine it with metformin which acts as an insulin sensitizer and reduces androgen levels in PCOS and gonadotropins. If oral drugs do not work then you give injections for stimulation and then you could go into laparoscopy and then into IUI or IVF. So, these are the drugs which cause the egg formation, correct the hormones, myoinositol which also correct the hyperandrogenism, hyperinsulinism.
I believe the young couples with suspected tubal block, endometriosis and coexisting PCO, ovaries and the duration of infertility is less than 2 years and semen analysis is normal , you do a laparoscopy and ovarian drilling. With this the androgen levels will go down, the hormonal level improves, automatic ovulation will start along with it you wash the uterus (hysteroscopy) and tubes are flushed, if there are small clots, mucus. It’s a very good fertility enhancing procedure, takes about an 1hr, it’s a keyhole surgery, good options for young patients, especially those who have not responded to medicines and do not want to go ahead with other ART methods.
And then of course there is IUI where you give either the medications or gonadotropins, you monitor. Of course natural intercourse is good even on superovulated cycle but if you time it specially in PCOS and wash it and inject it around the time ovulation the pregnancy rate with IUI in PCOS is definitely higher than natural. It can be tried in younger patients with good semen parameters or moderately low semen parameters.
When the age of the lady is high (usually more than 35 yrs) or tubal factor or male factor, or other methods are failing and she is not responding to low dose gonadotropins, you need to give high dose and if you have to give high dose you cannot do natural or IUI because of multiple pregnancy so you do the stimulation to take out the eggs, fertilization, embryo formation and transfer. Roughly in a good center it is about 50-55% pregnancy rate per embryo transfer and cumulative 2-3 cycle close to 90%, especially in young patients. So, IVF is one of the last option but really effective in women with PCOS. Earlier we worried about OHSS in PCOS, but with the antagonist protocol and agonist trigger the incidence of OHSS is close to zero.
PCOS needs a multidisciplinary effort. Lifestyle , fertility counseling, psychological support, nutritional counseling, metabolic intervention but finally overall the prognosis is good if lifestyle parameters are followed well and fertility potential and fertility prognosis is also very good.
https://pubmed.ncbi.nlm.nih.gov/14688154/
https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Polycystic-Ovary-Syndrome
The treatment of PCOS at Advance Fertility in India involves a comprehensive and personalised approach. Our skilled team of fertility specialists develops individualized treatment plans that, if necessary, incorporate medication, lifestyle changes, and assisted reproductive technologies. We aim to optimise fertility outcomes and enhance the general health and well-being of individuals afflicted with PCOS by addressing the underlying factors that contribute to the condition.
Dr. Kaberi Banerjee is distinguished as the best doctor for PCOS in Delhi due to her extensive experience and expertise in reproductive medicine. She is a dependable option for people looking for the best PCOS care in Delhi because of her tailored approach to patient care, dedication to staying current with innovations, and history of effective PCOS treatments.
Advance Fertility addresses the unique challenges of PCOS by tailoring treatment approaches to each individual’s specific needs. Our all-inclusive PCOS treatment programs may involve dietary recommendations, hormone-regulating medication, lifestyle changes, and, if required, advanced reproductive therapies.
Yes, PCOS can be effectively treated with lifestyle modifications at Advance Fertility. To control symptoms and enhance general health, our strategy combines dietary recommendations, consistent exercise, and other lifestyle modifications. A holistic treatment plan that addresses the underlying causes of PCOS and increases the likelihood of natural conception frequently includes lifestyle modifications.
Medication plays a crucial role in the treatment of PCOS at Advance Fertility in India. To control other PCOS-related symptoms, induce ovulation, or regulate hormonal imbalances, our fertility specialists may recommend medication. These drugs are specifically chosen for each patient based on their unique requirements, with the goal of helping PCOS patients conceive more successfully by reestablishing hormonal balance.
We care for each one who come to us with hope in their hearts.

Disclaimer – Dr Kaberi is not associated with any Hosptial/Clinic other than “Advanced Fertility and Gyne Center (AFGC)”. AFGC has only four centers at present 1. “Lajpat Nagar” 2. “CR Park Delhi” 3. “Noida” 4. “Gurgaon“.