Fertility Tests – Male

Semen analysis represents the most basic evaluation of the male infertility. The evaluation of the semen is based on the standards defined by the World health organization (WHO) for the laboratory manual for the examination and processing of the human semen. WHO gives the basic procedural standardization and reference values worldwide.
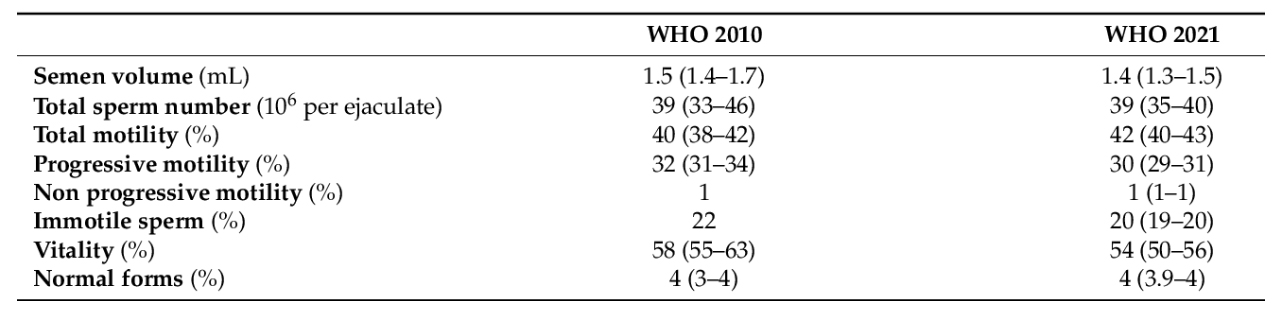
WHO 2010 (5th Edition) and WHO 2021 (6th Edition) lower fifth percentile (with 95% confidence interval) of semen parameters from men in couples starting a pregnancy within one year of unprotected sexual intercourse leading to a natural conception.
From the first edition in 1980 to the latest edition in 2021, there have been significant advances with incorporation of recent developments in the semen examination techniques.
The 5th edition aimed at standardized semen analysis procedure with step-by-step approach to basic to optimal test. This edition also added semen cryopreservation which plays an important role in fertility preservation & ART. It also added sperm processing for testicular and epididymal sperm. It added a lot in male infertility practice both from clinical and research purpose along with the reference ranges.
The 6th edition aimed to optimize semen analysis procedure by adding detailed steps. The 6th edition contains result of 3589 fertile subjects who took ≤ 12 months for time to pregnancy (including 1800 subjects from 5th edition). An important difference is abonnement of reference ranges in current edition.
Below are the some of the adjustments done in the basic sperm examination:
- Evaluation of the Semen odour which is subjective which makes it more complicated as it goes against the rules of personal protection against the viruses emerging.
- Readoption of progressive motility in two categories (A+B). the categorization is now Rapid progressive, slow progressive, non-progressive and immotile, without any recent studies showing its usefulness in the routine diagnosis.
- Semen dilutions have been simplified for calculating the semen concentration but 200 sperms should be counted. Low sperm count of <2mill/ml must be precisely counted and noted as it may lead to errors.
- The sperm vitality showed inconsistency with that of 5th edition. In current edition it is recommended when total sperm motility is below 40% but in previous edition it was done when progressive motility was below 40%, but 40% threshold itself corresponds to the total motility.
- Sperm morphology is explained systematically with multiple and better-quality micrographs in unprocessed sperm samples. Significance of Large cytoplasmic droplets are emphasized. Terms like normozoospermia, asthenozoospermia, teratozoospermia, necrozoospermia are voluntarily removed as the reference thresholds alone are meaningless and multiple criteria must be applied to establish a diagnosis in male infertility.
- Sperm DNA integrity is very important for proper embryo development, implantation, and pregnancy and in the 6th edition it is emphasized that SDF testing could represent an important addition in the work-up of male infertility.
Advanced Semen Analysis is a technique in which apart from the basic sperm parameters like, volume, viscosity, pH, sperm concentration, motility, and morphology other parameters like sperm motion kinetics are also assessed with computer aided sperm analyzer. It is an automated analysis of seminal fluid.
Normal sperm analysis is done by a trained technician easily who will assess the sperm concentration, number of motile spermatozoa and the morphology i.e., no. of normal form of spermatozoa, but when it comes to the sperm kinetics like curvilinear velocity, straight line velocity, amplitude of lateral head displacement, amplitude of lateral height it is possible only with the advanced technique like computer aided sperm analysis.
The advanced sperm test is an indicator of male reproductive health and in patients with unexplained infertility it may give a higher accuracy test then a manual sperm analysis. The patient gets a visual on the sperm parameters and is able to better understand his condition.
Sperm DNA Fragmentation Index is the amount of damaged DNA caused due to environmental or lifestyle factors or due to increased chromosomal aberrations, immature chromatin or aneuploidy in the spermatozoa. Sperm DNA integrity is very crucial for the fertilization and development of a healthy baby. Defective maturation or oxidative stress may lead to morphologically poor sperms which are associated with high amount of DNA fragmentation.
The DNA fragmentation score is usually determined through specialized laboratory tests such as the sperm chromatin structure assay (SCSA) or terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay. These tests analyze the integrity of DNA strands in sperm cells and provide a quantitative assessment of DNA fragmentation.
The test is not recommended for all and is usually done for patients with unexplained male infertility, varicocele, recurrent pregnancy loss , failed IVF and recurrant IVF failures.
If your result falls within 0 – 31%, you are within the fertile range. If your result falls between 31 – 100%, you are outside of the fertile range and have an increased risk of infertility.
Treatment like anti-oxidant therapy to control oxidative stress, antibiotic therapy for infection control like leukocytospermia, varicocelectomy, lifestyle changes may give better results with high DNA fragmentation Index.
Retrograde ejaculation is a condition in which semen is redirected into the bladder instead of being expelled through the urethra during ejaculation. It can be caused by various factors such as certain medications, nerve damage, or surgery.
When analyzing urine in men with retrograde ejaculation, the focus is typically on the presence of sperm in the urine. This is done through a process called urine sediment analysis or post-ejaculatory urine analysis. Here’s an overview of how it is usually performed:
- Collection of urine sample: The individual is asked to provide a urine sample shortly after ejaculation. This can be done by masturbating and collecting the urine sample immediately afterward. Alternatively, a urine sample can be obtained by using a special condom or a non-spermicidal condom with a collection bag during sexual activity.
- Laboratory analysis: The urine sample is sent to a laboratory for analysis. The lab technician will examine the urine sediment under a microscope to look for the presence of sperm cells. They will typically use a high-power magnification to increase the chances of detecting any sperm that may be present.
- Evaluation of sperm presence: If sperm are found in the urine sample, it confirms the diagnosis of retrograde ejaculation. The concentration and quality of the sperm can also be evaluated to determine the extent of the condition. The absence of sperm in the urine sample suggests that retrograde ejaculation is not the cause of infertility, and further investigation may be necessary to identify other potential factors.
Endocrine evaluation – This is a very aspect of analysis of male infertility especially azoospermia. Follicle stimulating hormone (FSH) levels help to decide whether the problem is at the synthesis level or duct level and whether hormone therapy will be useful. Testosterone / Estradiol hormone ratio sometimes help in deciding which medication will be preferred.
Ultrasonography – This helps in assessing testicular volume ,location , presence of any collection or varicocele.
Genetic Analysis
- Karyotype analysis : This test examines the number and structure of chromosomes in an individual’s cells. It can detect chromosomal abnormalities, such as Klinefelter syndrome (XXY), Y chromosome microdeletions, or translocations. These abnormalities can have a significant impact on sperm production and function.
- Y chromosome microdeletion analysis : This test specifically focuses on the Y chromosome, which contains genes essential for male fertility. Y chromosome microdeletions can be associated with impaired sperm production or complete absence of sperm (azoospermia). The test checks for the presence or absence of specific regions on the Y chromosome that are crucial for sperm development.
- Single gene mutation analysis : Certain genetic mutations can affect sperm production, sperm function, or hormone regulation, leading to male infertility. Tests can be performed to identify mutations in specific genes, such as the CFTR gene (associated with cystic fibrosis), the androgen receptor gene (associated with androgen insensitivity syndrome), or the SYCP3 gene (associated with spermatogenic failure).