Need Help?
We are here to help.
We care for each one who come to us with hope in their hearts.

Original Research Paper Published on Journal of Human Reproductive Sciences
Unconsummated marriage are mainly due to vaginismus or erectile dysfunction. They contribute to about 5% of couples in an infertility clinic. Their incidence is increasing in the metropolitan cities because of stressful lifestyles. Many of couples are advised intrauterine insemination as fertility treatment. However, home insemination is a simple, inexpensive and effective way of achieving pregnancy in such couples. We present the first study to document pregnancy rates of artificial home intravaginal insemination in couples with unconsummated marriage. Aim: To assess the pregnancy rates (PR) with intravaginal insemination (IVI) by couples with nonconsummation of marriage. Setting: Infertility outpatient clinic, New Delhi. Design: Retrospective analysis. Material and Methods: 55 couples of unconsummated marriage were evaluated in a period of two years. Group 1 contains 29 patients aged between 20 to 33 years; group 2 includes 14 patients aged between 33 to 36 years and group 3 includes 12 patients aged more than 36 years. Result(s): Unconsummated marriage was caused by vaginismus in 67% of the cases, erectile dysfunction in 22% and premature ejaculation in 11%. Clinical pregnancy rate was 69% in group 1; 43% in group 2 and 25% in group 3 after 6 cycles of AI. Conclusion(s): Intravaginal insemination is a simple, short, economical, effective and painless procedure for conception in nonconsummation of marriage.
Unconsummated marriage (UCM) is a disorder, in which couples are not able to achieve penile-vaginal penetration despite regular attempts in a certain period. Vaginismus and dyspareunia in females, erectile dysfunction (ED) and premature ejaculation (PE) in males, or combination of these factors are known to play major roles in the etiology. It is a common medical and social problem facing medical practitioners in conservative communities. It accounts for up to 17% of visits to sexual health clinics.[1] Vaginismus has been reported as a leading cause for UCM. In vaginismus, there is a spasm of the paravaginal muscles sufficient to prevent penile entry or to make it uncomfortable.[2] ED (or impotence) and PE are the two most prevalent complaints in male sexual medicine. ED is the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance.[3] Epidemiologic studies of ED suggest that approximately 5%–20% of men have moderate-to-severe ED.[4] PE is characterized by ejaculation which always or nearly always occurs before or within about 1 min of vaginal penetration and inability to delay ejaculation on all or nearly all vaginal penetrations and negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy.[5] PE is a common male sexual dysfunction, with prevalence rates of 20%–30%.[6],[7]
In all these factors, the couple faces difficulty in conception. However, they can be easily treated with a simple and painless procedure of artificial insemination (AI) by vaginal route. It is a simple and noninvasive technique, which can be performed without expensive infrastructure.[8]
This is the first study to the best of our knowledge that presents the pregnancy rates (PRs) of home artificial vaginal insemination in couples with UCM.
During the period from November 2014 to September 2016, 55 couples of UCM were evaluated with their informed consent. The study was carried out at our center. The patients were divided into three groups according to the age. Group 1 contains 29 patients aged between 20 and 33 years, group 2 includes 14 patients aged between 33 and 36 years, and group 3 includes 12 patients aged more than 36 years. UCM was assigned when a married male patient experienced failure of penile intromission into his wife’s vagina. All couples had been evaluated through history taking, physical examination, and constructed questionnaire. They underwent complete physical examination that focused on external genitalia and secondary sexual characteristics. A semen analysis with 3-day abstinence was performed. A transvaginal ultrasound was also performed to rule out any pelvic pathologies such as fibroids, polyps, and ovarian cysts. After this initial evaluation, the nature of the problem and different management options were discussed with the couple. All other causes of male and female infertility were excluded in the study.
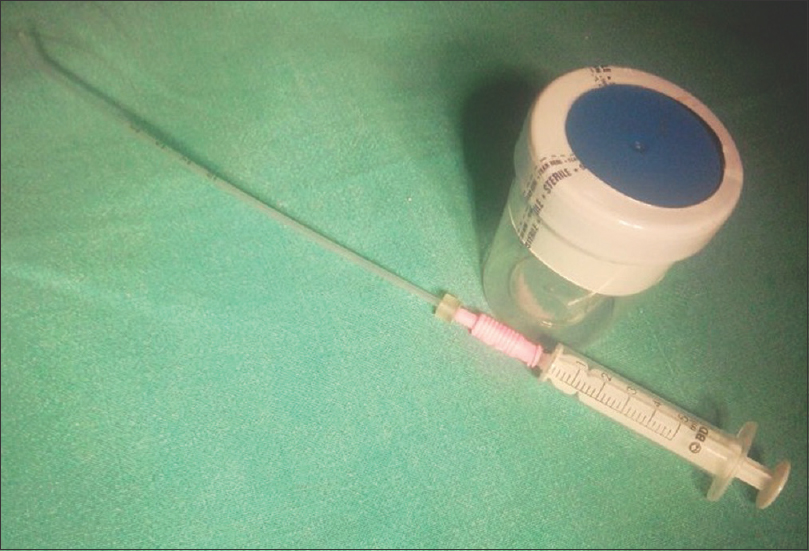
The AI kit contains a sterile semen container, a soft plastic intrauterine insemination (IUI) catheter, and a 5 cc syringe. The male partner was asked to collect the semen sample by masturbation in a sterile plastic semen container. The 5 cc syringe was attached to the IUI catheter and the guard was pulled completely to the distal end of IUI catheter. The IUI catheter was put in the sperm container and with negative suction entire sample was aspirated in the 5 cc syringe. The female partner was asked to lie down in the supine position with flexed legs and pillow the bottom in a private room. The husband was asked to insert the IUI catheter with attached syringe with loaded semen in the direction of 45° angle from the floor, and the husband was asked to inject it slowly inside the vagina and the patient was told to rest for 20 min after the procedure. This procedure of intravaginal insemination (IVI) was demonstrated to the couple once in the outpatient department.
They were asked to perform the same at home on every alternate day in the fertile period of female for six cycles. The semen was placed in the vagina with the help of the 5 cc syringe attached to the soft IUI catheter to facilitate semen deposition deep into the vagina [Figure 1]. After the insemination, the female was advised to lie in the same position for ½ h to prevent any seepage of semen. The couples were asked to return when the urine pregnancy test was positive or there was no result in six cycles.
A total of 55 couples complaining of UCM were retrospectively included in the study. The age of the female partners was 20–40 years. The duration of marriage in all the age groups was 1–7 years, with average duration of 3.5 years, and the same is applied for the duration of infertility. In the first age group, average duration of marriage was 2.5 years with range of 1–5 years.
The etiological factors underlying the UCM are illustrated in [Table 1]. [Table 2] depicts the age distribution and the average number of insemination cycles in each group.
Table 1: Etiological factors of unconsummated marriage

Table 2: Group characteristics
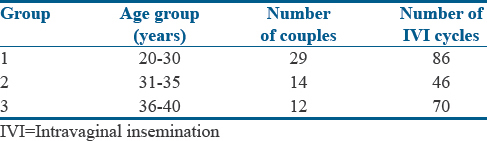
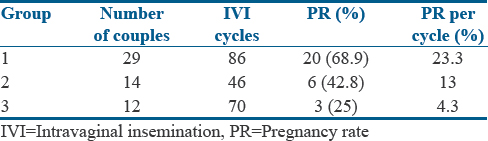
During this period, in 55 women, 202 cycles of intravenous immunoglobulin (IVI) were performed. Each woman had 1–6 IVI cycles. In group 1, 86 cycles were done in 29 women; in group 2, 46 cycles of IVI were performed in 14 women, and in group 3, 70 cycles were done in 12 women. In an average, three cycles were done in group 1, four cycles in group 2, and six cycles in group 3. Women aged 20–40 years were inseminated and there was age-related decline in PRs. The PR which was recorded as the positive urine pregnancy test according to age group is depicted in [Table 3].
Table 3: Pregnancy outcome of intravaginal insemination
Artificial vaginal insemination is an assisted conception method that can be used to alleviate infertility in selected couples. This is the first study to document the clinical PRs using artificial vaginal insemination in nonconsummation of marriage to the best of our knowledge.
Nonconsummation can be due to vaginismus, ED, or PE. There are treatments available for them such as vaginal dilatation, hymenectomy, behavioral therapy, or urological intervention.[8],[9] However, many couples are resistant to these treatment and suffer from chronic nonconsummation for as long 10–15 years.[8],[9] Fertility is a major concern for many of them.
Most of them are advised to go through IUI after failed attempts at vaginal dilatation and medical treatment for ED. However, IUI is more invasive. The woman may not allow Cusco speculum insertion and may even need general anesthesia for the same. It needs more visits to the doctor and the clinic, thus imposing on day-to-day life. It is more expensive as it involves sperm preparation, ultrasound monitoring, and hospital visits.
Artificial home vaginal insemination on the other hand is simple and inexpensive and does not require repeated hospital visits. It maintains the privacy of the couples. It has good pregnancy results especially in young ovulatory couples with open tubes and good sperm parameters.
It may be argued that IUI has better chances of conception than IVI and therefore should be a preferred mode of treatment. Although there are no studies comparing pregnancy outcomes of home IVI to IUI in couples with nonconsummation, there are some studies comparing peri- or intra-cervical insemination to IUI in women undergoing donor sperm insemination. Drenth et al. in 1996 have mentioned self-insemination as a bedroom procedure to be a means to procreate in women with vaginismus where penetrative intercourse is not an option.[10] They however have not documented the PRs. The Cochrane study in 2008 confirms IUI to have better pregnancy outcome.[11] The study showed that IUI after six cycles significantly improved live birth rates (odds ratio [OR] 1.98, 95% confidence interval [CI] 1.02–3.86) and PRs (OR: 3.37, 95% CI: 1.90–5.96) in comparison to cervical insemination. A large study in 2015 found no difference in PRs in women undergoing IUI or cervical insemination (CI) of donor sperm.[12] Cumulative PRs up to six treatment cycles were 40.5% for IUI and 37.9% for CI. Kathiresan et al. have compared pregnancy outcomes by IVI and IUI in 82 couples with male factor due to infertility due to spinal cord injuries. They found the results to be comparable.[13]
We therefore present the first study documenting the pregnancy outcome of artificial home IVI in couples with UCM. We conclude that home vaginal insemination is a patient-friendly cost-effective way to get such couples pregnant.
Home insemination is a simple, patient friendly and cost effective way to get pregnant for couples suffering from unconsummated marriages.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
We care for each one who come to us with hope in their hearts.

Disclaimer – Dr Kaberi is not associated with any Hosptial/Clinic other than “Advanced Fertility and Gyne Center (AFGC)”. AFGC has only four centers at present 1. “Lajpat Nagar” 2. “CR Park Delhi” 3. “Noida” 4. “Gurgaon“.