Need Help?
We are here to help.
We care for each one who come to us with hope in their hearts.

Q1. A young couple is unsuccessfully trying to conceive from the past 5 months. In which patient would you suggest ART and in whom will you advice to conceive normally.
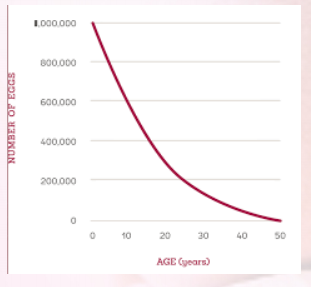
a. Young couples who are trying to conceive for less than two years and in whom all other parameters (hormonal profile, TVS, tubal patency and semen analysis) are normal can wait and continue trying naturally. However women with bilateral tubal damage, ovarian failure and poor endometrium will need IVF/third party reproduction soon rather than later. Men with poor sperm count or azoospermia will need IVF/ICSI with or without TESA.
Since the results of fertility treatment are age dependent any woman who has received unsuccessful treatment for more than 3 years or who is more than 35years of age should avail soon rather than later
Q2.A 28yr.old lady married for 5yrs with primary infertility and bilateral tubal block undergoes IVF.10 eggs are retrieved, 7 get fertilized and 6 good quality embryos are transferred. How many embryos will you transfer? What is your opinion about single embryo transfer?
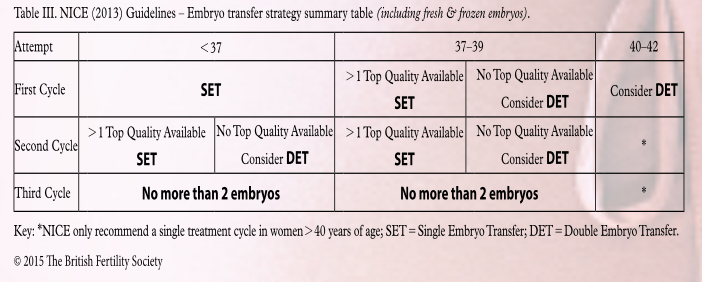
The Following table shows the number of embryos that can be transferred according to NICE guidelines.
The ASRM( in April 2012) society recommends-
The Utilization of eSET has increased over the past decades in the U.S. Use Of ET has also increased but the twining rate has remained the same. eSET is most
appropriate for those with the good prognosis. Elective SET is most appropriate for those with the good prognosis age <35 years more than one quality embryo available for transfer, first or second treatment cycle, previous successful IVF and recipients of embryos from donated eggs.Women aged 35-40 years may be considered for eSET if they have top quality blastocyst-stage embryos available for transfer.Decisions regarding eSET of cryopreserved embryos should take into consideration prognosis, embryo quality and success rates of the individual cryopreservation program. Challenges to increased use of eSET exists. These include provider and patient education, financial consideration, embryo selection and successful cryopreservation .Stake holders should recognize that the optimal outcome of an IVF cycle is the birth of the healthy singleton. Reduced financial burdens for IVF through insurance coverage or risk sharing programs have been shown to improve patient acceptance of eSET. Selection and successful cryopreservation of the embryos with the highest IRs(implantation rates) will facilitate wider use of eSET.
De Sutter at all in an original paper title ‘Does three or more embryos make sense for a well defined population of infertility patients undergoing IVF/ICSI/?’In
obstetrics and gynecology general in 2012 discuss the need to transfer more number of embryos in a select group of patients. Table 1 describes the Belgian policy.
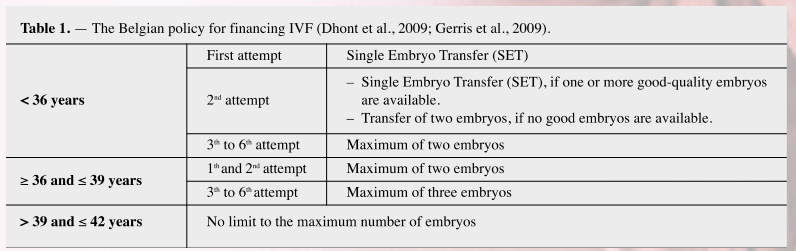
The paper analyzed the relation between the probability of outcome and the number of embryos transferred.
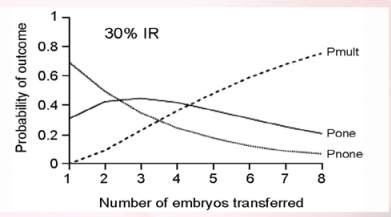
The paper then suggests a clinical protocol where HLT (more than three embryos)will be a good option.
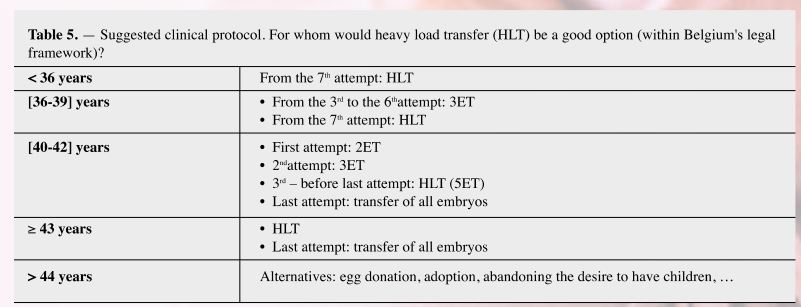
The paper suggests that HLT can be considered for the poor prognosis group of women. Limiting the number of embryos to transfer to a maximum of two in all
cases probably leads to under treatment of this subpopulation. Facts Views Vis Obgyn. 2012;4(1):51-518
In India IVF is an uninsured medical process. Patients pay out of their own pockets and they usually come at an advance age for IVF. The ovarian reserve in South Asian population is 2-3 yrs advance in Caucasian. Endometritis is also common. Considering all these parameters transfer of two or more embryos may be justified in certain situations. In the Indian scenario eSET can only be done in young good prognosis patients and in labs having robust cryopreservation system.
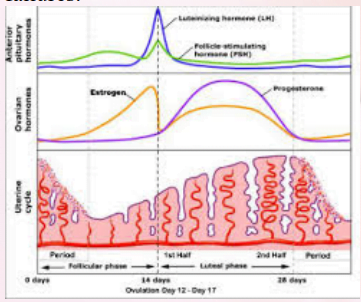
Q3. What is the recommended luteal phase support in first trimester in IVF pregnancies?
a. Luteal phase support is needed in IVF pregnancies because during follicular aspiration there is disruption of granulosa cells which leads to compromise corpus
luteum. Supra physiological concentration of steroids secreted by high number of follicles also demands increase progesterone support .Progesterone can be taken in
oral, vaginal or intramuscular form.
Micronized progesterone can only be taken as vaginal, rectal or intra muscular form. Recent studies have indicated that oral dydrogesterone is a viable alternate to
micronized progesterone .
Human Reproduction.2018,1;33(12):2212
HCG or progesterone given during the luteal phase may be associated with higher rates of live birth or ongoing pregnancy than placebo or no treatment, but the
evidence is not conclusive. The addition of GnRH at o progesterone appears to improve outcomes. hCG may increase the risk of OHSS compared to placebo.
Moreover hCG with or without progesterone, is associated with higher rates of OHSS than progesterone alone. Neither the addition of estrogen nor the route of
progesterone administration appears to be associated with an improvement in outcomes.
Cochrane DatabaseSyst Rev.2015 Jul 7;(7):CD009154
The addition of estrogen in Luteal phase is beneficial.
JBRA Assist Reprod.2017 Sep 1;21(31):247
Addition of other adjuvants like aspirin can be given in specific situation like antiphospholipid antibody syndrome, thrombophilia and recurrant implantation
failures.
Q4. Pregnancy has reached 12 weeks: what next?
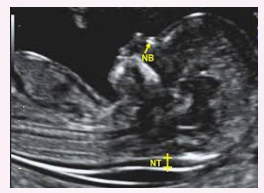
i. First trimester screening – ultrasound (Down syndrome markers, early anomaly scan, uterine artery Doppler) + serum biochemistry.
a. Combined screening (USG for NT/NB and dual marker) has the highest detection rate for Down syndrome. Adding Placental growth factor (PlGF) to the dual marker has the added advantage of screening women for the risk of developing early preeclampsia/fetal growth restriction – early identification allows starting low dose aspirin at the correct gestation.
ii. Any different in twins or higher order multiples?
a. Combined screening (USG + dual) has the best detection rate for twin pregnancy as well.
b. MoMs need to be corrected for both IVF and chorionicity.
c. A single risk is assigned for monochorionic twin pregnancies.
d. Individual risks are calculated for each twin in dichorionic pregnancy.
e. No role of dual marker in higher order multiples.
f. Quadruple marker in twins has detection rate of only 56% and should be done only when first trimester screening has been missed.

iii. Serum biochemistry in twins with one vanishing twin
a. If fetal pole and cardiac activity seen – treat as twin. If empty sac – treat as singleton.
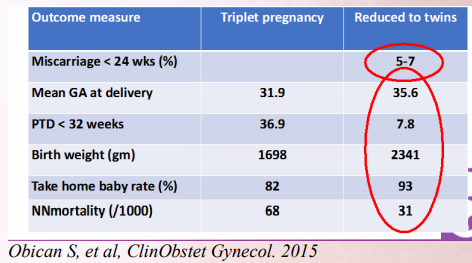
Q5. What should we do when we are faced with higher order multiple pregnancy ?
i. Reduction versus expectant management
a.5-7% risk of procedure related miscarriage (per fetus reduced)
ii. Triplets with one monochorionic pair – whom to reduce?
a. Ideally reduce the monochorionic pair because of 10-15% risk of twin twin transfusion syndrome (TTTS) and/or selective FGR (7% risk of miscarriage). Interstitial laser if couple wants to have twins (10% risk of procedure related miscarriage, another 50% risk of losing the cotwin after 2 weeks).
Q6. How is Antenatal follow up in twins?
i. Monochorionic versus dichorionic
a. Monochorionic: 2 weekly ultrasound surveillance, delivery at 36-37 weeks. Dichorionic: 4 weekly ultrasound surveillance, delivery at 37-38 weeks.
ii. Higher order multiples
Weekly ultrasound surveillance, delivery at 34-36 weeks.

iii. Role of bed rest
No role! Detrimental – increased risk of DVT and adverse outcomes. Restricted activity may be advised.
Q7. Prevention of preterm labour in twin pregnancy?
i. Role of progesterone.
a. Though there are no robust randomized controlled trial (RCT) studies, most studies have indicated the benefits of progesterone in IVF twin pregnancies. BJOG. 2017 Jul;124(8):1163
On the basis of current knowledge, progesterone should be offered to women with a documented history of a previous spontaneous birth at less than 37 weeks and for those found to have a short cervical length of 15mm or less. Studies are needed to evaluate progesterone efficacy on other risk factors.
Curr Opin Obstet Gynecol. 2009 Apr;21(2):142
ii. Role of routine cervical screening
a. Routine cervical length screening may reduce the risk of very preterm birth. Journal of Obstetrics and Gynaecology. 2018 March 14;(38):789
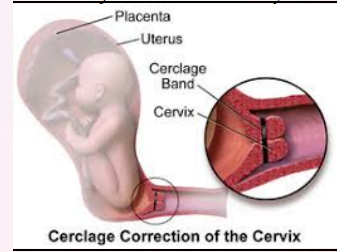
iii. Role of prophylactic cerclage
Cerclage works in a carefully selected group of patients. Recent studies have indicated that routine prophylactic cerclage even without shortening may be beneficial. Ultrasound Obstet Gynecol.2016 Nov;48:752-756
iv. Role of antibiotics
a. The evidence supports not giving antibiotics routinely to women in preterm labour with intact membranes in the absence of overt signs of infection. Further
research is required to develop sensitive markers opf subcilical infection for women in preterm labour with intact membranes, as this is a group that might benefit from future novel interventions, including new modalities of antibiotic therapy. The results of this review demonstrate the need for future trials in the area
of preterm birth to include assessment of long-term neurodevelopmental outcome. Cochrane Database Syst Rev. 2013 Dec 5;(12):CD000246
Q8. Role of Antenatal steroids ?
i. Routine prophylaxis?
a. No benefit if >7 days elapse from steroid cover –
no role of routine prophylaxis
ii. At what gestation?
Anytime upto 34 weeks when preterm labour (iatrogenic or spontaneous) Benefit proven even upto 36 weeks (ASTEROID trial) when preterm delivery. Elective LSCS – upto 39 weeks
iii. Role of second (rescue) dose?
ACOG – if >2 weeks have elapsed and gestation is less than 34 weeks, one rescue dose may be given.
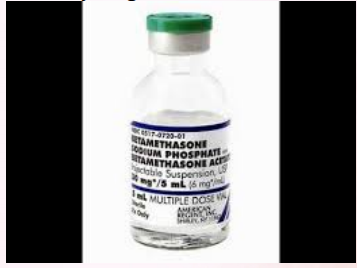
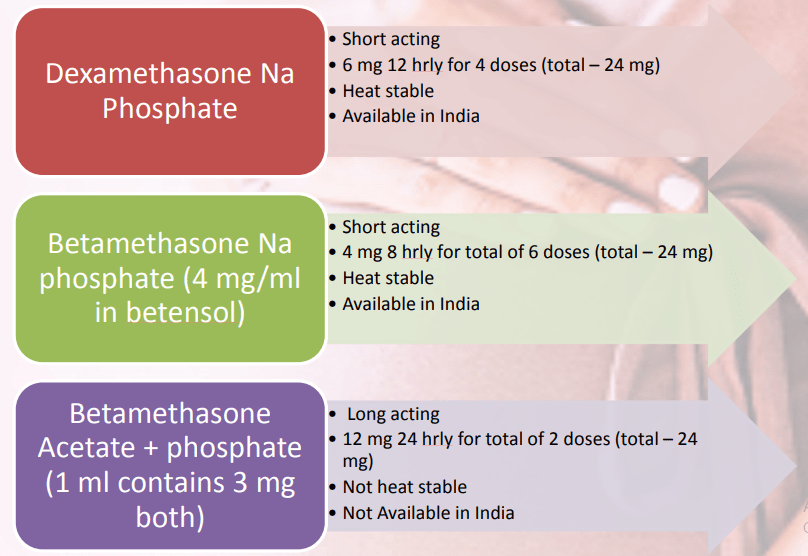
iv. Which steroid and what dose? Dexa versus betamethasone
a. Dexa versus betamethasone
GOI 2014 – dexamethasone (beta salt AA, dexa less susceptible to heat)
v. Role of Tocolysis
Should be considered for steroid cover.
At Advance Fertility and Gynecology Centre ,New Delhi, Dr. Kaberi Banerjee recommends prophylactic steroid cover at 26-28 weeks and repeat course at 30-32
weeks for all multiple pregnancies. This way early preterm delivery is covered. None of the babies deliver with such a regimen of steroid cover required extended
neonatal ICU Care or surfactant treatment ,even in cases where delivery is at 30-32 weeks of gestation.
Q9. At what gestation should an IVF pregnancy be referred to a tertiary care centre?
If high risk factors develop (either maternal or fetal), in utero transfer is better than delivery and transferring the neonate.
Low threshold for transfer at gestations less than 34 weeks.
Q10. Multiple pregnancy: optimal time for delivery? Twins : Dichorionic versus Monochorionic.
Timing of delivery-Dichorionic Twin Pregnancy
• Depends on chorionicity
• Uncomplicated dichorionic/diamniotic twin – 38 – 38+6 weeks
• Delivery at 37 to 37+6 wks is reasonable alternative
• Earlier if complicated by Intrauterine growth restriction
Obstet Gynecol. 2016;128(4):e131
Timing of delivery-Monochorionic Twin Pregnancy
• Diamniotic monochorionic
• Before 36+6 wks
BMJ. 2016;354:i4353
ACOG suggests
• Uncomplicated monochorionic – 34 – 37+6 wks
• If growth restricition – 32 to 34+6
Obstet Gynecol. 2016;128(4):e131.
• Monoamniotic monochorionic
• Delivery early in third trimester

• Select your patient group for ART carefully.
• Judgement the number of embryos to be transferred is multifactorial.
• Luteal phase support is helpful in first trimester.
• Addition of Adjuvants must be done on a case to case basis.
• Select your patient group for ART carefully.
• Judgement the number of embryos to be transferred is multifactorial.
• Luteal phase support is helpful in first trimester.
• Addition of Adjuvants must be done on a case to case basis.
• IVF Pregnancies do need special care.
• Prophylactic Steroids-There is role of prophylactic steroids and cerclage in IVF twin
pregnancies.
• Cerclage.
• In Utero Transfer of extremely premature babies well equipped neonatal I.C.U. is always
preferred.
• Role of good NICU cannot be over emphasis in handling IVF pregnancies.
We care for each one who come to us with hope in their hearts.

Disclaimer – Dr Kaberi is not associated with any Hosptial/Clinic other than “Advanced Fertility and Gyne Center (AFGC)”. AFGC has only four centers at present 1. “Lajpat Nagar” 2. “CR Park Delhi” 3. “Noida” 4. “Gurgaon“.